learning center
Living with MSA
Multiple System Atrophy presents unique challenges to patients and their families that require lifestyle adjustments. Mission MSA is dedicated to easing this transition by offering resources to help patients assemble their care teams, effectively manage symptoms, and explore potential clinical trials.
Please Note:
The information on this website is intended for general informational purposes only, and is not a substitute for professional medical advice, diagnosis, or treatment. The information on this website may not be suitable or applicable to your medical condition or health goals. You should always consult with a qualified medical professional before making any decisions or taking any actions that may affect your health.
Your Care Team
Due to the rare nature of this disease and the complexity of its symptoms, many MSA patients see a multitude of providers before receiving their diagnosis. It is imperative to receive timely and informative medical care from a multi-disciplinary team when treating and managing symptoms.
Below is a list of potential members of a multi-disciplinary care team and what they may recommend or help you with, but your exact needs will vary.
Movement Disorders Specialist
Movement Disorders Specialist
Occupational Therapists
Occupational Therapists
Physical Therapists (PTs)
Physical Therapists (PTs)
Registered Dietitians (RDs)
Registered Dietitians (RDs)
Social Workers
Social Workers
Speech Language Pathologists (SLPs)
Speech Language Pathologists (SLPs)
Therapists / Counselors
Therapists / Counselors
Urologists
Urologists

Movement Disorder Specialists
Visit the International Parkinson and Movement Disorder Society’s directory to find local providers for your care team.
Symptoms & Treatment Options
The premotor phase of MSA can last for months to years. Patients may present with a combination of symptoms, but will likely not experience all of the symptoms listed above. A diagnosis of definite MSA is not possible until the postmortem examination is performed. However, research has allowed for advances in diagnostic assessments to aid in clinical diagnosis and enhance patient care.
Symptom presented at onset may be motor or non-motor
- Sexual dysfunction
- Urinary dysfunction
- Retention or incontinence
- Sleep disturbances
- REM Behavior Disorder (RBD): Shouting or thrashing while asleep, acting out dreams, sleep walking
- Sleep apnea or snoring
- Autonomic symptoms
- Neurogenic Orthostatic Hypotension (nOH): Lightheadedness, dizziness, or passing out when changing positions from lying to sitting or sitting to standing
- Reduced sweating
- Significant changes in blood pressure
- Cold extremities, specifically hands and feet
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua.
Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Excepteur sint occaecat cupidatat non proident, sunt in culpa qui officia deserunt mollit anim id est laborum.
- Stridor
- high pitched sound while breathing
- Parkinsonism symptoms
- tremors and/or feeling slow and stiff when moving
- Cerebellar symptoms
- imbalance and feeling unsteady or clumsy
- Subtle changes to voice and speech
- slower and quieter and/or slurred
- Difficulty writing
- small and spidery handwriting (micrographia)
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua.
Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Excepteur sint occaecat cupidatat non proident, sunt in culpa qui officia deserunt mollit anim id est laborum.
- Pyramidal signs
- spasticity, weakness, slowing of rapid movements on one or both sides of the body
- Recurrent falls
- need for walking devices
- Coughing while eating and drinking
- Need for indwelling or intermittent catheterization
- Difficulty turning in bed
- Unintelligible speech
- need for communicative devices
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua.
Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Excepteur sint occaecat cupidatat non proident, sunt in culpa qui officia deserunt mollit anim id est laborum.
- Reduced appetite and weight loss
- Inability to verbally communicate
- Shallow or bubbly breathing
- Need for gastrostomy
- Need for tracheostomy
- Potential for aspiration Pneumonia
- Potential for uroseptic fever
Progression & Prognosis
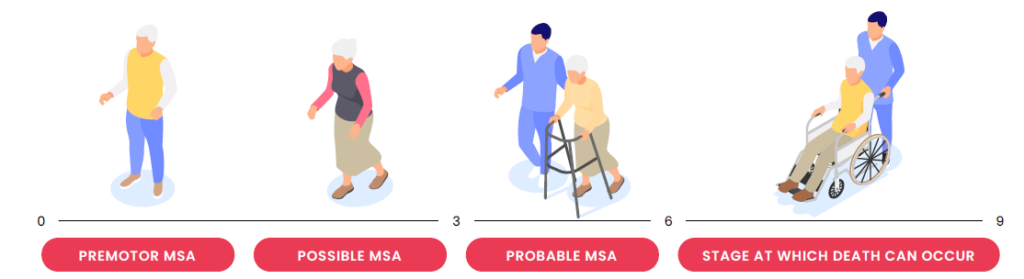
The progression of MSA is relatively gradual and linear, with most patients passing away from the disease or its complications within 6-10 years after the onset of symptoms. Since MSA goes through multiple stages, it is extremely important to keep in contact with your care team and update them on your symptoms or any changes you may be experiencing. While there is currently no treatment or cure for MSA, many of its symptoms are manageable with drug and non-drug therapies.
Contact our Support Line at (866) 737-5999.

Non-Drug Therapies
While there is currently no cure for MSA, various non-drug therapies can help manage symptoms and improve quality of life. Explore a list of some non-drug therapies commonly used in the management of MSA.

End of Life Planning
At some point in your MSA journey, you will need help with your everyday needs. Whether that is a loved one who can serve as a care partner, or hiring a healthcare professional, it is vital to have a care team lined up to assist you and/or your family.
Centers of Excellence
Additional Resources

Resource Library
Explore Mission MSA’s extensive collection of digital and downloadable resources including videos, infographics, brochures, and more in the MSA Resource Library. Utilize these resources to gain a deeper understanding of the aspects of MSA impacting your life.
